As telehealth solutions become more sophisticated, public health agencies are re-thinking how to manage health devices.
Telehealth is booming. While the concept of providing health services over the internet is not new, it has been turbo-charged by the COVID-19 pandemic and related restrictions.
Back in Grandma’s day, telehealth meant using the telephone to make an appointment with the doctor. Now the doctor can visit over the Zoom screen, but this is really just one small part of telehealth. Today’s telehealth addresses multiple stages of a health engagement, and beyond.
Key areas include:
- Consultation
- Typically a video call between patient and clinician. Useful in general terms only, as anything specific would require observational data.
- Observational diagnostics
- This is what a clinician normally acquires during an examination. With telehealth, this requires testing & monitoring devices at the patient’s premises.
- Monitoring
- This can be done via health monitoring devices which remotely deliver data to the clinician, and can provide alerts to either the clinician or the patient or both.
Delivering telehealth is not trivial. Having a nice app is good, but by itself does not address some of the key needs.
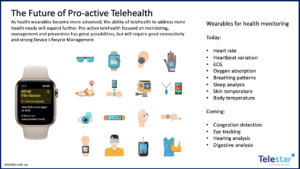
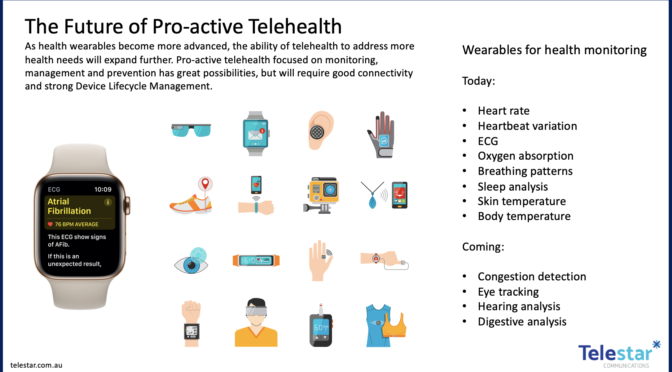
Central to the expansion of telehealth is the concept of monitoring and data collection. Various devices have been available in this area for many years now, ranging from “medic alert” necklaces for the elderly that provide remote monitoring in case of a fall, up to sophisticated IT wearables such as smart watches, smart glasses and smart clothing that offer everything from heart rate and sleep analysis right through to electrocardiograms and skin temperature measurements.
As this area heats up, the innovations are arriving at a rapid pace. Apple is rumoured to be enhancing its Airpods product to also measure the wearer’s temperature, while Tytocare is even trying to provide both custom diagnostics devices and the doctors at the end of the videocall all in one bundle.
But there are also two significant limitations on today’s telehealth:
- IT wearables today do not address some key diagnostic and monitoring needs, including blood pressure (as opposed to heart rate), body temperature and sample/swab testing.
- A significant number of citizens do not have the personal technology to take advantage of telehealth, because of unfamiliarity with tech, and/or lack of interest, and/or socio-economic circumstances.
For both public health agencies and insurers, these limitations suggest a need for a pro-active approach. Around the developed world, this typically involves the agency or insurer shipping a “kit” of monitoring and communications gear to selected patients. Kits typically include a number of connected medical devices for self-observation as well as a smart tablet for aggregating the data and for communication during a telehealth consultation. Kits are designed to be simple to use, and accessible for the elderly and for those unfamiliar with modern personal tech.
This approach is very effective, but is obviously very expensive. For this reason, it is typically used only for particularly at-risk patients and often only during a finite “period of concern”.

COVID-19 has increased the appeal of this ‘ship-a-kit’ approach to telehealth, with public health agencies from Bavaria to Singapore to northern Japan using it on their most at-risk or infected citizens. Patients can be monitored efficiently and comprehensively without needing to leave their home, thus minimising the risk of virus spread. When a patient recovers or is no longer at-risk, the kit is collected, physically cleaned, data-wiped and re-configured for the next patient.
The enabling capability for this type of telehealth is Device Lifecycle Management (DLM).
Unlike simple online shopping where goods are delivered and (sometimes) returned, DLM involves both the physical logistics and the software and data aspects of device setups, communications setups, accounts, security and data resets.
Unlike simply ordering a new phone, DLM involves the staging of the mobile devices as well as the kitting of the special medical accessory devices.
And unlike just managing work-from-home IT packs for new employees, DLM involves managing the devices and accessories to health standards throughout a device lifecycle that may include many dozens of different patients for each kit, as well as secure storage and management of the device and accessory pool between uses.
Some systems will break, some devices will fail, and some accessories may even be damaged by patients themselves. Managing the timely replacement and repair of kits so that service is not interrupted is also a key part of DLM.
Finally, DLM needs to be manageable. The service needs to provide asset registration as well as detailed spend reporting, all centralised and easily digestible, so that public agencies have full control and visibility of both the CAPEX and OPEX spend as they go.
Telehealth offers enormous benefits for public health in the future, As telehealth evolves, the promise of more efficient and pro-active telehealth services will become reality for many more people. Expanding telehealth beyond what is offered by consumer IT devices, and ensuring the service can reach those citizens without access to their own technology, will be a key priority for all public health agencies.
At the implementation level, the foundation of this is DLM.